Professional hockey player Rich Peverley gave a news conference today in which he and his medical team announced surprising details about his heart condition.
We learned that atrial fibrillation and its treatment featured prominently in his collapse during a game earlier this week.
“A flare-up last week led Peverley to skip a road game, and he had upped his medicine.”
Here is an email I received from another journalist:
“They’re saying he was diagnosed with atrial fibrillation when he was traded in the offseason and went for a physical. The procedure was that they “shocked” his heart. The plan was to do an ablation but they wanted to wait until the offseason because of the amount of time he would miss. They said the plan was made in conjunction with Peverley himself, his agent, the team and the team medical staff. The procedure was performed at the Cleveland Clinic.
They said it only took 14 seconds before they began the medical response, which they had planned for. They think on Monday he was somewhere between atrial fibrillation and atrial flutter when they shocked him.”
That last sentence is tough to understand. In twenty years of practice, I have seen only two possible ways a healthy patient (without WPW) could collapse from AF or atrial flutter. One is 1:1 flutter from a Type Ic drug (flecainide or propafenone); the other is polymorphic VT (torsades de pointes) from a Type III drug (sotalol, dronedarone, dofetilide or amiodarone). In this case I favor the former. The teaching point is that he likely suffered a pro-arrhythmia from an AF drug.
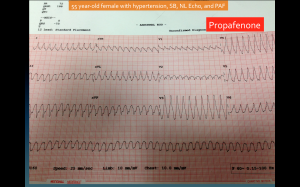
Earlier this month I posted this picture of 1:1 flutter recorded from a patient taking propafenone. At over 250 beats per minute, you can see how it might cause collapse.
This news sheds light on the ongoing debate concerning the treatment of atrial fibrillation, especially in athletes.
It also strengthens my thesis that one of the greatest dangers faced by AF patients is AF treatment.
This story has direct implications about what should (or could) be first-line treatment for AF. Should patients with AF have to fail medical therapy before having catheter ablation? There are skeptics who question the use of AF ablation. They point to the procedure’s significant risks, invasive nature, modest success rates, thin evidence base and big costs. These are all appropriate concerns. But make no mistake: AF drugs are not exactly benign either.
I’m working on more of the (teaching) details, so stay tuned.
My aim is not to invade the privacy of Mr. Peverley. I think we can work with what he and his team have released thus far to form a narrative that will inform both patients and doctors.
That said, this is really good news for Mr. Peverley. Suffering a complication of AF treatment is far better than having a primary ventricular arrhythmia or heart muscle disease (cardiomyopathy).
And this too: the diagnostic details of what may have caused his collapse does not diminish the benefit of early intervention by bystanders. Quick and effective response to those who collapse from heart rhythm disturbances remains an important public health matter.
JMM
22 replies on “Atrial fibrillation features prominently in Rich Peverley collapse”
Okay, so you’re saying Peverly may have had the cardiac incident because his medication was increased? This would slow the heart down even further? I had an ablation 4 months ago and now take Sotolol. I am in sinus rytham since. After 5 cardio versions prior, the ablation seems to have worked. I am athletic and find it difficult to raise my heartbeat now because of the Beta Blocker. But in two months I’m going to half the Sotolol dosage. Would like to know more about the Peverly case and how a-fib could cause cardiac arrest (which I did not think probable). Thanks.
Read this http://www.drjohnm.org/2013/08/atrial-flutter-15-facts-you-may-want-to-know/ specifically #7. Also> look up torsades de pointes.
I had surgery to correct WPW…not sure if this was what Mr. Peverly had or not…but I am fine now. Surgery was the best decision I made as I too would get heart flutters since I was a child that would make me feel light headed and start sweating. I could actually tell when the flutters were going to start ie. after/during certain types of activities or conditions.
The doctors found this out in a way similar to what happended to Mr. Pevely. I was playing soccer and almost passed out during a heart flutter episode. I went to the ER directly after the game and they found the abnormal rythum on the EKG.
It has been approx. 8 years since surgery. I take no meds and I feel great. Just somehting to think about if you are considering surgery or not.
Just to clarify… The team doctor said he was in v-tach and vfib.
“Medically, it’s a little difficult for the doctors to pin down precisely what happened, as they were focusing mostly on reacting and only had a small rhythm strip once they attache the AED to go off of. Dr. Dimeff said that strip indicated Peverley’s heart was bouncing between two abnormal and extremely dangerous rhythms, ventricular tachycardia and ventricular fibrillation.”
Link:http://www.defendingbigd.com/2014/3/12/5501486/dallas-stars-rich-peverley-collapse-heart-press-conference-season-over-ablation-CPR
That’s one reporter’s take of an orthopedist’s take.
Look at that ECG I showed in the post. 98/100 non-electrophysiologists would call that 1:1 flutter a VT. It’s a hard diagnosis for a cardiologist to make, nevermind an orthopedist or a medic on the scene.
But even if it was VT/VF, my teaching point remains. Young people with AF–he had a normal heart muscle and no coronary disease–don’t collapse unless they take medicine for the heart rhythm.
This is not a knock on his docs. Any electrophysiologist has seen this. It happens. It’s well documented in clinical trials. Athletes are especially prone to pro-arrhythmia b/c the nature of sport is to push oneself to extreme levels of exertion.
Good points.
Thank you!
Joe
To echo Dr. M. as a paramedic I would call that ECG VT without thinking twice, and treat it as such. I would actually love to know what you look for to distinguish the ECG above as 1:1 A-flutter. I’ve been following the Peverley case with interest both as a hockey fan and a medic, and also believe that it could raise the profile of the chain of survival for out of hospital SCA.
s a little difficult for the doctors to pin down precisely what happened, as they were focusing mostly on reacting and only had a small rhythm strip once they attache the AED to go off of. Dr. Dimeff said that strip indicated Peverley’s heart was bouncing between two abnormal and extremely dangerous rhythms, ventricular tachycardia and ventricular fibrillation.
http://www.defendingbigd.com/2014/3/12/5501486/dallas-stars-rich-peverley-collapse-heart-press-conference-season-over-ablation-CPR
Hey Dr. John a questions which is bothering me and it seems the source you mentioned may be wrong as in this source it says he had vtach and vfib. So as you said in this article do you feel for the most part that the medication he was taking to prevent a fib and keep his heart in sinus rhythm was the culprit for the vfib? Otherwise outside of meds in <35 yr old patients isn't only possibility of Vfib from some heart abnormality i.e. myopathy.
sorry just saw a previous made statement by a fellow reader was the exact same!
Very nice post Dr. John, but i am a little perplexed as although it can cause him to collapse do these Type I Meds with great possibilities of pro-arrythmias potentially cause Cardiac Arrest as well? it did with this individual Peverley for a few seconds in most articles I have read, so can the proarrythmias which in this case caused by a Type 1 med cause such a possibility?
Dr. John:
Can you explain in plain English what you think occurred here? In your post you say:
“The teaching point is that he likely suffered a pro-arrhythmia from an AF drug.”
But then in your reply to David Matthews comment, you directed him to an article on atrial flutter.
I’m thoroughly confused. Are you saying you think he collapsed due to his afib medicine or from atrial flutter…or are you saying his afib medicine likely caused atrial flutter…which led to the collapse?
Travis
http://en.wikipedia.org/wiki/Proarrhythmia
causes existing arrythmias to reoccur at possibly greater occurrence due to medication. Ironic i know.
Dr. John:
I’m confused. In your post you say:
“The teaching point is that he likely suffered a pro-arrhythmia from an AF drug.”
But then in your reply to David Matthews comment, you directed him to an article on atrial flutter.
Are you saying you think he collapsed due to his afib medicine or from atrial flutter…or are you saying his afib medicine likely caused atrial flutter…which led to the collapse?
I only ask for the clarification because I quoted you in my latest blog post and would like to better understand your analysis:
http://www.livingwithatrialfibrillation.com/627/dallas-stars-rich-peverley-out-for-season-due-to-atrial-fibrillation/
Dr. John:
I’m confused. In your post you say:
“The teaching point is that he likely suffered a pro-arrhythmia from an AF drug.”
But then in your reply to David Matthews comment, you directed him to an article on atrial flutter.
Are you saying you think he collapsed due to his afib medicine or from atrial flutter…or are you saying his afib medicine likely caused atrial flutter…which led to the collapse?
I only ask for the clarification because I quoted you in my latest blog post and would like to better understand your analysis:
http://www.livingwithatrialfibrillation.com/627/dallas-stars-rich-peverley-out-for-season-due-to-atrial-fibrillation/
Travis
Doc John,
This scares me. I have afib as well as VT and was put on sotolal a couple of months ago due to my very high heart rate that was occuring due to the afib. I had been on Flecanide prior to that due to numerous episode of extreme nausea while playing hockey. I’ve always been very active and my docs have encouraged me to do so.
Looks like I will be having another discussion with my EP doc.
Linda
Mr. Peverly’s collapse reminds me of my own. Two years ago, after my second ablation, I was prescribed a combo of diltiazem and flecainide to treat AF and atypical flutter. Soon after my first dose, while bike commuting to work, I suddenly blacked-out and crashed. No one had warned me about possible side-effects. Can’t wait for the results of the proposed study of the Comparative Effectiveness of Treatment Options for Atrial Fibrillation in Athletes.
Dr. John:
I’m confused. In your post you say:
“The teaching point is that he likely suffered a pro-arrhythmia from an AF drug.â€
But then in your reply to David Matthews comment, you directed him to an article on atrial flutter.
Are you saying you think he collapsed due to his afib medicine or from atrial flutter…or are you saying his afib medicine likely caused atrial flutter…which led to the collapse?
I only ask for the clarification because I quoted you in my latest blog post and would like to better understand your analysis:
http://www.livingwithatrialfibrillation.com/627/dallas-stars-rich-peverley-out-for-season-due-to-atrial-fibrillation/
Travis
Prior to my AF ablation when I was experiencing an Afib episode, I sometimes would feel suddenly like I was about to blackout. I think this was due to a long pause between heartbeats (something that was noted when a wore a monitor for 3 weeks). The sensation may have also been triggered or agravated by anxiety. In any case, I did actually collapse a few times from this sensation.
Back when I was still in Afib (on Amiodorone and a beta blocker) I keeled over while playing a very low key game of tennis. Didn’t lose consciousness, but it knocked me off my feet. It seemed to resolve itself after about 10 minutes of rest, but I was done for the day.
If I had to do it all over again (and no thank you, I would rather not) I would push harder for an ablation rather than going through so many futile rounds of medications (3 of them) and electrocardioversions (8 of those). It took three attempts, but the ablations were the only treatment that made any lasting difference.
Organized atrial tachycardia or atrial flutter (Is it just a semantic difference?) often present with a ventricular beat being triggered for every second or every third atrial beat. Treatment with flecainide can reduce the likelihood of episodes. However, break-through tachycardia while on flecainide can result in each beat being conducted through, one-for-one. Too much strain for ventricles. Which is why metoprolol is paired with flecainide just for this contingency. It slows everything down to a less dangerous rate.
This is my electrophysiologit’s explanation.
Trouble is, the treatment slows EVERYTHING down and QoL suffers – all for the contingency.
Greetings. Very educational article. My daughter had WPW masked by SVT when she was 5 years and had it corrected by catheter ablation back in 2001. I kind of ran with the theory that the Peverley thing was WPW when I heard the initial reports. Apparently not?
What concerns me about their course of action was not just his playing and not the conclusion that they would have people onsite during the games “just in case.” I think they rolled some ugly dice with his life and got extremely lucky that his incident didn’t happen while behind the wheel of a car or by himself in the whirlpool bath or several thousand feet in the air on a plane. I realize that there are potential dangers with ablation, as with any surgery, but would argue in favor of the ablation over any medical treatment currently out there. It seems to me the risks of simply treating with medication vastly outweigh any risk associated with ablation. I’m glad he is okay, but I am very disappointed by the medical advice he received.
Totally agree with your informed take on AF antiarrhythmic drugs being dangerous.
I am a 64 year old female overweight former endurance cyclist with lone afib, and no other health problems and a generally low BP and HR.
A few weeks ago I was going through a stressful period and began having afib episodes at about 2 per week after having no episodes for seven months prior.
The EP offhandedly gave me Flecainide “pill in the pocket” (300mg) with no warning whatsoever of possible side-effects.
It worked twice, and then the third time sent me to the hospital two and a half hours away with rampaging atrial flutter, which fortunately self-converted before they could zap me.
I am to see this guy again in a couple of days and want to clean his clock, but also don’t want to antagonize him (in case he does my ablation.)
Why don’t EP’s routinely warn of possible trouble with these scary drugs??
Why isn’t that part of the protocol?
My other problem is I have tried several times to access your article on Atrial Flutter, but it seems to be in perpetual maintenance mode.
(Just FYI…)
I LOVE your blog and Medscape stuff.
The medical profession needs to hear what you are saying.
Perhaps you have room in your AF ablation queue for one more out of state old lady patient…(I’m not joking!)