As a descriptive word, Electrophysiology sounds over-complicated. When introducing myself to patients, I almost always refer to myself as a heart-rhythm specialist. Other doctors call us “EPs.”
EP–a much easier name–is a branch of cardiology that deals with the diagnosis and treatment of heart rhythm disorders. We do an extra year (or two) of training after the standard cardiology fellowship.
EP doctors do three things:
- Ablate (Burn or freeze)
- Implant and manage cardiac devices.
- Take care of patients.
Ablate:
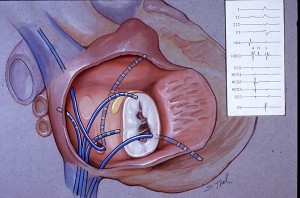
 Catheter ablation is a procedure in which a small catheter is placed inside the heart (via a leg vein). The catheter has a 4-8 mm metal tip through which radio-frequency (or cryothermal) energy is delivered to selected parts of the heart. (The area to ablate is selected primarily by two simple strategies: vector analysis of the how the arrhythmia activates the heart (ie…north-south, east-west) and secondly, by moving the ablation catheter in a “warmer-colder” trial-and-error manner.) The 4-8 mm ablation lesions can eliminate rogue cells that have electrically run amok, or in the case of AF, isolate areas of the heart.
Catheter ablation is a procedure in which a small catheter is placed inside the heart (via a leg vein). The catheter has a 4-8 mm metal tip through which radio-frequency (or cryothermal) energy is delivered to selected parts of the heart. (The area to ablate is selected primarily by two simple strategies: vector analysis of the how the arrhythmia activates the heart (ie…north-south, east-west) and secondly, by moving the ablation catheter in a “warmer-colder” trial-and-error manner.) The 4-8 mm ablation lesions can eliminate rogue cells that have electrically run amok, or in the case of AF, isolate areas of the heart.
Catheter ablation is the only cardiac procedure that can be correctly called curative. (No, stents do not cure atherosclerosis.)
I learned ablation in the mid-1990s but did not start using it for atrial fibrillation until 2004. Over the past few years, AF-ablation has emerged as electrophysiology’s most exciting therapy. Here is a link to my atrial fibrillation page.
Devices:
The other procedural aspect of electrophysiology is implantation of cardiac devices. Pacemakers, Defibrillators (ICDs) and Cardiac Resynchronization Therapy (CRT=BiVentricular) are placed under the skin in the upper chest and are connected to wires that are snaked through veins and positioned into the heart for sensing, pacing and shock delivery.
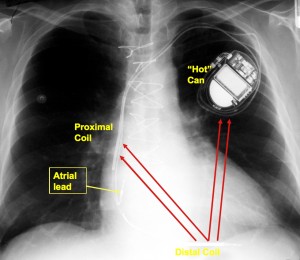
Although it takes time to learn the surgical installation process, and attention to detail to do it well, the far greater challenge in device management is skillfully applying these complex therapies in the management of patients–the judgment part.
In a selected group of patients, ICDs lower the risk of death. They are, however, associated with substantial risk to the patient. Here is the link to my ICD/Pacemakers archives. Also of interest are these posts on ICD complications. (I urge those interested in understanding the limitations of the ICD trials to read, Mark Josephson’s Critical Appraisal of ICDs in JACC-2008
Doctoring:
Electrophysiologists are not just proceduralists and installers. We are real medical doctors.
In many cases, a heart rhythm problem results from a random event–a fluke. Supra-ventricular tachycardia (SVT), lone-AF in a young healthy person, and congenital AV-block are just three examples of many such hiccups of nature. These non-acquired (congenital) problems comprise a substantial portion of our practice. EP doctors are fortunate because we get to treat a wide range of patients: from the very young, with congenital disease, to the aged with the disease of excessive birthdays, and everywhere in between.
In other cases, the heart’s rhythm is affected by environmental factors, both cardiac and non-cardiac. For instance, hardening of the arteries and heart attacks cause heart rhythm problems. So does long-standing high blood pressure, diabetes, sleep disorders and bad lifestyle choices.
Understanding whether to use a catheter, a device, a medicine, or in some cases, none-of-the-above, requires us to listen to, exam, and talk with our patients. In other words…be a doctor. The verb for this is doctoring, which I write about frequently. (Tags of archived posts similar to doctoring are at: ‘Joy of Medicine,’ medical-decision making, and General Medicine.)
Electrophysiology is a beautiful field because it mixes pharmacology, procedures, and old-fashioned doctoring to help people.
JMM
2 replies on “What’s Electrophysiology?”
[…] Tell them that there are specialists that spend almost their entire day (minus the time it takes for paperwork, clicking the e-chart and doing time-outs) treating AF. We are called electrophysiologists. […]
[…] a doctor who works in a field–electrophysiology–that is almost exclusively preference-sensitive, I’ve grown increasingly interested in […]